Thermography: Safer and Earlier Detection of Breast Cancer
AUTHOR Annette Chlumsky, RN
Thermography has been a controversial detection tool for breast cancer for quite some time. It has been used since the 1960s; however, the cameras back then were not very sensitive and therefore not as reliable as they are now.
Thermography in 2016 has a vastly improved heat-sensing scanner technology using highly sophisticated infrared cameras that make over seventy-six thousand digital measurements with each image. In addition, the field of thermography has developed an extensive scientific clinical research data bank of over 800 published research papers, that includes the testing of more than 300,000 women. This has helped the field of thermography to gain ground among more progressive practitioners.
Even though there is reliable technology existing today, there is limited awareness and insufficient education. This has resulted in the underuse of thermography in clinical practice. In 1981 the FDA listed breast thermography as an adjunctive diagnostic procedure for breast cancer and reaffirmed this position in 1998. The National Cancer Institute lists breast thermography as a diagnostic procedure for breast cancer detection and described it as “probably the earliest indicator for breast cancer.”
Breast thermography measures differences in infrared heat emission from normal breast tissue, benign breast abnormalities (such as fibrocystic disease, cysts, infections and benign tumors) and breast cancer. It does this with a high degree of sensitivity and accuracy. It is a non-invasive measurement of the physiology (function) of the breast tissue, rather than the anatomy (structure) which other imaging such mammography, sonograms, and MRIs may identify.
Tumor tissue does not have an intact sympathetic nervous system and therefore it cannot regulate heat loss. When the breast is cooled in a room kept at 68 degrees Fahrenheit, blood vessels of normal tissue respond by constricting to conserve heat while tumor tissue remains hot. Thus, tumors emit more heat than their surrounding tissues and are usually more easily detected. As the disease progresses, cancerous tissues stay hot, they do not cool down. In contrast, other conditions such as fibrocystic breasts, infections, inflammation disorders cool down as they resolve.
Breast thermograms find highly specific thermal patterns in each individual woman. They provide a unique “thermal signature” that remains constant over years unless there is a change in an underlying condition. For this reason it is important to have a benchmark early in a woman’s life, beginning at age 25. Then, over time it is possible to differentiate between cancer and benign conditions.
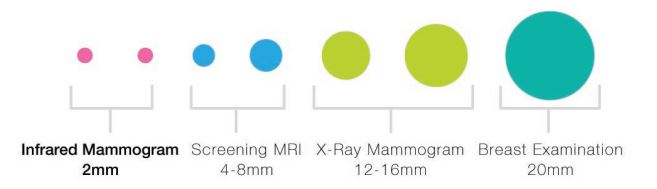
Most breast cancers do not become palpable until they are larger than one centimeter and often by that time 25% have already metastasized. Thermograms detect changes that precede breast cancer. An asymmetrical increase in temperature is a diagnostic sign. At least five studies published between 1980 and 2003 document that thermal imaging is a major advancement in identifying breast cancers, not only with greater sensitivity and specificity, but also years earlier than with any other scientifically tested medical technology. False-positive results are a criticism of breast thermograms; however, the positive result may actually be a forewarning indication of developing malignancy, warning of tissue changes that precede breast cancer, but cannot yet be picked up on radiological or ultrasound imaging.
Mammography has been the state-of-the-art screening test for several decades. However, considerable controversy remains regarding its value, particularly in women under the age of 50. For younger women, mammography is more likely to miss the aggressive breast cancers that are typically diagnosed in this age group, especially in women with dense breast tissue who are at a significantly increased risk for developing breast cancer. For women between the ages of 40 and 44, breast cancer is the leading cause of death according to the American Cancer Society. Thermography is more sensitive for recognizing abnormalities in the younger and/or denser breast tissue. Other difficulties in reading mammograms can occur in women who are on hormone replacement therapy, nursing, fibrocystic, large breasted, or with breast implants. These situations are compatible with thermography which is more diagnostically sensitive.
Many women have avoided mammography screenings because of years of accumulating radiation exposure. Thermography provides an alternative screening option for women who may not have agreed to a screening mammogram. Breast thermography involves no radiation exposure or breast compression, is as easy to do as standing in front of the infrared camera, and is affordable.
Generally accepted breast cancer risk factors for which screening is particularly important are:
• having started your first period before age 12
• having gone through menopause after age 50 
• having your first child after age 30 or never pregnant
• on hormone replacement therapy or birth control pills
• consuming one or more alcoholic drinks per day
• having a family history of breast cancer
• having the inherited breast cancer gene
• postmenopausal
• postmenopausal weight gain
• sedentary lifestyles
• elevated insulin levels and type 2 diabetes.
Riordan Clinic uses Therma-Scan Reference Laboratory, which is the most experienced breast thermography facility and has been in business since 1972. Thermograms are graded with a system much like pap smears with grades 1-5. TH1 and TH2 are normal, TH3 is moderately abnormal, and TH4 and TH5 are severely abnormal. If the thermogram report comes back with a significant high score, patients are referred for further evaluation. We use thermography as a screening tool and an adjunct to other modalities- mammography, ultrasound and MRI.
You do not need to be a patient to schedule a thermogram at RC. If you are not a patient, and the results are of concern, you may discuss it with a nurse and take the report to your doctor. If you are a patient, and results are indicative of an abnormality, your doctor will be available for a consult to develop a nutritional program to help reverse the inflammation or atypical pattern, attempting to prevent a more serious disease process.
To schedule an appointment for breast thermography, please call 316.682.3100